Connect With Us
Blogs

Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Unraveling the Causes of Bunions
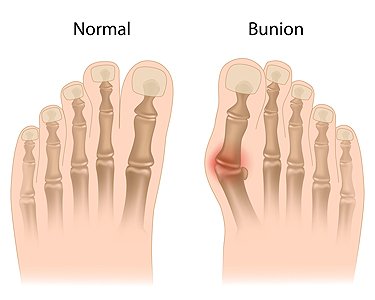
Bunions, also known as hallux valgus, are bony bumps that form at the base of the big toe. This condition occurs when the big toe pushes against the adjacent toe, causing the joint to move out of alignment. There are various reasons why bunions can develop. Genetics play a significant role, as individuals with a family history of bunions are more likely to develop them. Wearing ill-fitting shoes, especially those with narrow toe boxes, can exacerbate the condition. As bunions progress, symptoms become more pronounced. Common signs include pain, swelling, redness, and stiffness around the affected joint. Corns and calluses may develop due to friction from overlapping toes. As a bunion worsens, the shape of the foot may change, possibly affecting balance and walking patterns. Early detection and appropriate measures, such as wearing supportive footwear and using padding or orthotic inserts, can help manage symptoms and prevent further deformity. If you have a bunion, it is strongly suggested that you visit a podiatrist who can provide you with relief and treatment options that are right for you.
If you are suffering from bunions, contact one of our podiatrists of Redwood Podiatry Group. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in Eureka and Arcata, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Definition and Causes of Foot Blisters

Blisters on the feet appear to be bubbles that are filled with liquid. This can cause irritation and can easily put a damper on our active lives. Understanding their causes can empower us to take better care of our feet. Foot blisters are small, fluid-filled sacs that form on the outermost layer of our skin, resulting from friction, pressure, or irritation. When our skin is subjected to repetitive rubbing against surfaces such as shoes or socks, it responds by separating its layers and accumulating fluid, forming a blister. Friction is the primary cause of foot blisters, especially when ill-fitting shoes or rigorous activities cause excessive rubbing. Additionally, prolonged exposure to moisture from sweat can weaken the skin's protective barrier, making it more susceptible to blisters. High temperatures can also exacerbate friction and contribute to blister development. By understanding the definition and causes of foot blisters, there are proactive measures that can be taken to prevent them. Properly fitting footwear, moisture management, and good foot hygiene can keep these bothersome blisters at bay, allowing us to stay active and comfortable on our feet. It is suggested that you consult with a podiatrist if you are seeking additional prevention techniques for blisters on the feet.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact one of our podiatrists of Redwood Podiatry Group. Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our offices located in Eureka and Arcata, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are pockets of fluid that occur under the top layer of your skin. These fluid pockets are usually filled with pus, blood, or serum. Blisters may itch or hurt and can appear as a single bubble or in clusters.
The most common types of blisters are friction blisters. This type of blister may be caused by wearing shoes that are too tight. Friction blisters can also occur on the hands. A change in temperature may also cause blisters on the feet. In the freezing air, frostbite on your toes can lead to blisters, as well as sunburn from hot weather.
The best way to treat a blister is to keep it clean and dry. Most blisters will get better on their own. Once the skin absorbs the fluid within the blister, it will flatten and eventually peel off. You should avoid popping your blister unless you podiatrist does it for you. Additional treatment options include applying an ice pack to the blister or using over-the-counter blister bandages to cover the affected area.
If your blister becomes discolored, inflamed, or worsens it is advised that you speak to your podiatrist. Blisters that are yellow, green, or purple may be infected and require immediate medical attention. Blisters that are abnormally colored may be a sign of a more serious underlying health condition such as herpes.
Stress Fractures in the Feet

Dancers and basketball players, as well as runners, may be familiar with stress fractures in the feet. This overuse injury, which consists of hairline fractures of the bones in the foot, often results from repetitive pounding on hard surfaces. A sudden increase in activity, such as playing longer and more often, or adding excess mileage to a run, can result in developing stress fractures. These tiny cracks are easy to dismiss at first because the pain often diminishes with rest. They also are difficult to detect with a foot X-ray, and often may only be noticed through digital imaging tests. Certain types of footwear, exercise equipment and surfaces, as well as insufficient rest periods are other major contributors to foot stress fractures. Finally, osteoporosis, arthritis, and neuropathy can be factors. A podiatrist can offer a clear diagnosis of stress fractures, and depending on the severity can offer the appropriate treatment options. For more information, it is suggested that you make an appointment with a podiatrist.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact one of our podiatrists from Redwood Podiatry Group. Our doctors can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
- Gender – They are more commonly found in women compared to men.
- Foot Problems – People with unusual arches in their feet are more likely to develop stress fractures.
- Certain Sports – Dancers, gymnasts, tennis players, runners, and basketball players are more likely to develop stress fractures.
- Lack of Nutrients – A lack of vitamin D and calcium may weaken the bones and make you more prone to stress fractures
- Weak Bones – Osteoporosis can weaken the bones therefore resulting in stress fractures
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact our offices located in Eureka and Arcata, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
Why Did I Develop an Ingrown Toenail?

An ingrown toenail is a common foot condition that can quickly become infected. This ailment is defined as the toenail growing into the skin instead of over it. It can happen for various reasons, including trimming the toenails incorrectly and wearing shoes too tight around your toes. Additionally, some people may have an abnormal nail structure or may have genetic tendencies toward developing an ingrown toenail. Common symptoms can consist of redness, extreme tenderness, and an infected nail may ooze pus. An ingrown toenail is generally a painful condition, and prompt medical attention is often sought for relief. Soaking the feet in warm water, followed by gently pushing the nail away with a small piece of cotton may bring temporary relief. If you have developed an ingrown toenail, it is suggested that you confer with a podiatrist who can provide you with permanent relief options and offer effective prevention methods.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact one of our podiatrists of Redwood Podiatry Group. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our offices located in Eureka and Arcata, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Is a Lateral Ankle Sprain?

A lateral ankle sprain is considered the most common type of ankle injury. This can happen when the ankle rolls inward and can affect the anterior talofibular and calcaneofibular ligaments. These ligaments are on the outside of the body and may become injured when the ankle moves past its normal range of motion. The common symptoms many people experience with an ankle sprain often include severe pain, swelling, and difficulty moving the ankle. It is beneficial to have a proper diagnosis performed, which consists of having an X-ray taken. This is successful in ruling out a fractured ankle, and treatment can begin for the sprained ankle. The affected ankle can be wrapped in an elastic bandage, and existing swelling may be reduced when the foot is elevated. If you have sprained your ankle, it is suggested that you confer with a podiatrist who can provide you with treatment options that are right for you.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact one of our podiatrists from Redwood Podiatry Group. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our offices located in Eureka and Arcata, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.







